 Living with chronic pain for virtually my entire adult life, I have tried almost everything I can think of to help manage it. My initial attempts to stoically tough it out and just push ahead resulted in months of near sleepless nights, constant pain, exhaustion and misery. Eventually, I began to tackle pain from both the Western medicine approach of pharmaceuticals, shots and surgery to the holistic and complementary medicine alternatives of acupuncture, chiropractic, naturopathy and massage. The more proactive I became—drastically changing my diet, reducing stress and listening to my body’s needs—the better I was able to manage the pain. When I finally fully embraced yoga and mindfulness meditation, I saw the greatest improvements in my health. New research from the National Institutes of Health (NIH) and the University of Texas helps to explain how yoga helps us heal from chronic pain, both physically and mentally.
Living with chronic pain for virtually my entire adult life, I have tried almost everything I can think of to help manage it. My initial attempts to stoically tough it out and just push ahead resulted in months of near sleepless nights, constant pain, exhaustion and misery. Eventually, I began to tackle pain from both the Western medicine approach of pharmaceuticals, shots and surgery to the holistic and complementary medicine alternatives of acupuncture, chiropractic, naturopathy and massage. The more proactive I became—drastically changing my diet, reducing stress and listening to my body’s needs—the better I was able to manage the pain. When I finally fully embraced yoga and mindfulness meditation, I saw the greatest improvements in my health. New research from the National Institutes of Health (NIH) and the University of Texas helps to explain how yoga helps us heal from chronic pain, both physically and mentally.
What’s the Matter With the Brain in Chronic Pain?
Yoga practitioners were found in NIH studies to have more grey matter in the cerebral cortex and subcortical areas of the brain than people with chronic pain. Grey matter is a type of tissue of the central nervous system that processes information in the brain, such as stimuli from sensory organs. The cerebral cortex plays a major role in perception, memory and attention.
“Imaging studies in multiple types of chronic pain patients show their brains differ from healthy control subjects,” M. Catherine Bushnell, PhD, scientific director of the Division of Intramural Research for the NIH, said at a recent meeting of the American Pain Society, according to Business Standard. “Our research shows that grey matter loss is directly related to the pain when we take depression into account.”
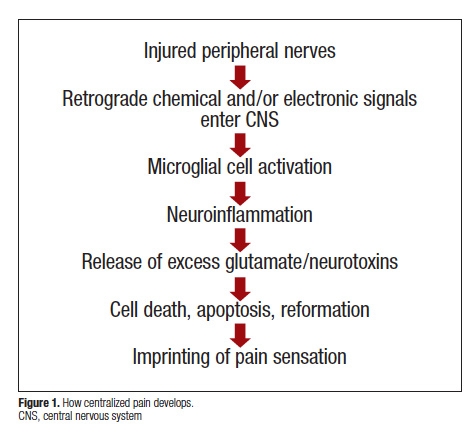 When a peripheral injury doesn’t completely heal, chronic pain can cause structural, functional and chemical changes in the brain, altering how it processes and modulate pain signals. The brain begins to generate abnormal levels of excitatory and inhibitory neurotransmitters–chemicals that relay signals between nerve cells, communicating information through the brain and body. Due to abnormal function in brain circuitry, many people with chronic pain have problems with autonomic responses and cognition, causing memory impairment and emotional issues. It is not uncommon for people with chronic pain to experience associated anxiety and depression.
When a peripheral injury doesn’t completely heal, chronic pain can cause structural, functional and chemical changes in the brain, altering how it processes and modulate pain signals. The brain begins to generate abnormal levels of excitatory and inhibitory neurotransmitters–chemicals that relay signals between nerve cells, communicating information through the brain and body. Due to abnormal function in brain circuitry, many people with chronic pain have problems with autonomic responses and cognition, causing memory impairment and emotional issues. It is not uncommon for people with chronic pain to experience associated anxiety and depression.
Bushnell said there is convincing evidence from numerous studies that mind-body techniques, such as yoga and meditation, can counteract the brain anatomy affects of chronic pain.
Yoga Helps Reverse Effects of Chronic Pain In the Brain
“Practicing yoga has the opposite effect on the brain as does chronic pain,” she said. “Some grey matter increases in yogis correspond to duration of yoga practice, which suggests there is a causative link between yoga and grey matter increases.”
A Harvard University-affiliated study Massachusetts General Hospital (MGH found that just a half hour of mindfulness meditation every day for eight weeks was enough to “stimulate a major increase in gray matter density in the hippocampus,” wrote MGH researcher Sue McGreevey.
“The encouraging news for people with chronic pain is mind-body practices seem to exert a protective effect on brain grey matter that counteracts the neuroanatomical effects of chronic pain,” Bushnell said.
Yoga is also believed to trigger endorphins, which act as a painkiller and reduce the perception of pain. Yoga also improves overall health by reducing chronic inflammation and stimulating the parasympathetic nervous system, helping to rebalance the body from the constant fight-or-flight response of chronic pain.
It is estimated that almost a third of the adult population in America, or 100 million people, suffer from chronic pain, according to a 2011 report from the Institute of Medicine. Chronic pain is medically defined as any pain in the body that lasts more than three months. When we suffer a peripheral injury, pain signals travel like electricity from the site of the injury to the spinal cord, triggering electrical or chemical signals to other cells, which are then relayed to the brain. When acute pain becomes chronic, nerve cells continue sending pain signals to the brain even in the absence of a persisting peripheral injury.
“Acute pain is important; it alerts the brain that there is danger. But for chronic pain, there is no separate system. It continually alerts the brain that there is something wrong, and yet it doesn’t stop. There is no way to calm it down,” physician turned mindfulness meditation teacher Christiane Wolf, M.D., Ph.D. told HuffPost Healthy Living.
A focal injury may lead to systemic pain that is increasingly complicated to manage and treat. The mechanism by which this occurs is unknown but researchers believe chronic pain changes how the multiple pain signals in the brain are activated.
Earlier this year, researchers at University of Berne in Switzerland also identified a brain mechanism that may be responsible for chronic pain. Scientists discovered that neurons in a region of the brain called gyrus cinguli change with chronic pain. Negatively stimuli constantly activate these excitable neurons, creating a type of “pain memory” that is difficult to stop.
More recent research by the University of Texas at Dallas found that the neurotransmitter dopamine, a chemical produced by the brain that is also associated with cognition, emotion and regulating movement, plays a significant role in chronic pain. The researchers found that removing a specific collection of nerve cells, or A11 neurons, containing dopamine significantly reduced selective chronic pain in mice, according to the study published in The Journal of Neuroscience.
“This may open up new opportunities to target medicines that could reverse chronic pain,” said the study’s senior author Ted Price, an associate professor in behavioral and brain sciences at UT Dallas.
“In future studies, we would like to gain a better understanding of how stress interacts with A11,” he added.
While stress is heightened with pain, pain also intensifies under stress. With the constant stress of chronic pain, muscles tense and tighten and breathing often becomes shallow and irregular. A focus on deep and controlled thoracic-abdominal breathing in yoga helps to fully oxygenate the body and shift it from fight-or-flight mode to relaxation.
How Mindful Meditation Helps Manage Pain
Yoga and mindfulness have proven helpful for deconstructing the process by which pain becomes chronic. According to Wolf, mindfulness can help people better cope with pain by removing the emotional and mental tension that can exacerbate physical pain.
“Nobody likes pain. But just because something is unpleasant doesn’t mean we have to suffer or react against it,” she said. A change of perspective can help a person better tolerate the experience of pain.
Wolf believes that the experience of pain is made up of the physical sensation, how we emotionally feel about it and the meaning pain holds for us. Key in the latter is learning how to once again separate pain from our personal identity. Mindfulness brings us into the present to see how we actually feel now, as opposed to being stuck in the trauma of the past—rehashing how my accident derailed my plans after graduation—or worrying over the potential limitations on our future—will I ever be able to teach full-time again?
“We start to see that the physical pain is separate from the emotions we feel about it,” Wolf said. “We describe the sensation. We label it. That awareness is what is helpful.”
Meditation has also been shown to play a role in modulating dopamine “the feel-good hormone” levels. An in vitro demonstration of the deeply relaxed, yet conscious state of Yoga Nidra meditation showed that there was a 65 percent increase in endogenous dopamine release, as well as decreased blood flood to the subcortical regions. Researchers at the University of Southern California also found that exercise helps the brain cells to use dopamine more efficiently.
Mind-body practices like yoga and meditation thus might play a key role in reducing the abnormal levels of excitatory and inhibitory neurotransmitters that trigger the chronic pain loop. For me, getting on the mat not only helps to physically release tension through stretching and strengthening; it also helps me to mentally focus my attention on something constructive that brings me into deeper body and breath awareness. The pain is no longer a foe I’m fighting, but a friend I am trying to help; the mind and body can feel the difference.

[…] our capacity to recover from injury and illness. Studies have shown that mindfulness meditation and yoga, for example, can stimulate an increase in grey matter density in the hippocampus to combat the…. Yoga, as well as other types of exercise, can also trigger endorphins, which can reduce the […]